Benign paroxysmal positional vertigo
From Wikipedia, the free encyclopedia
Benign paroxysmal positional vertigo (BPPV) is a disorder caused by problems in the inner ear. Its symptoms are repeated episodes of positional vertigo, that is, of a spinning sensation caused by changes in the position of the head.[1]
Classification
Vertigo, also called dizziness, accounts for about 6 million clinic visits in the U.S. every year, and 17–42% of these patients eventually are diagnosed with BPPV.[1] Other forms of vertigo include:
- Motion sickness: a disjunction between visual stimulation and proprioception
- Visual exposure to nearby moving objects (examples of optokinetic stimuli: passing cars, falling snow)
- Any other causes of vertigo – (labyrinthitis, Ménière's disease, migraine,[2] etc.)
Cause
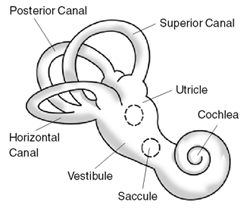
Within the labyrinth of the inner ear lie collections of calcium crystals known as otoconia. In patients with BPPV, the otoconia are dislodged from their usual position within the utricle and they migrate over time into one of the semicircular canals (the posterior canal is most commonly affected due to its anatomical position). When the head is reoriented relative to gravity, the gravity-dependent movement of the heavier otoconial debris (colloquially "ear rocks") within the affected semicircular canal causes abnormal (pathological) fluid endolymph displacement and a resultant sensation of vertigo. This more common condition is known as canalithiasis.
In rare cases, the crystals themselves can adhere to a semicircular canal cupula rendering it heavier than the surrounding endolymph. Upon reorientation of the head relative to gravity, the cupula is weighted down by the dense particles thereby inducing an immediate and maintained excitation of semicircular canal afferent nerves. This condition is termed cupulolithiasis.
It can be triggered by any action which stimulates the posterior semi-circular canal which may be:
- Tilting the head
- Rolling over in bed
- Looking up or under
- Sudden head motion
BPPV may be made worse by any number of modifiers which may vary between individuals:
- Changes in barometric pressure - patients often feel symptoms approximately two days before rain or snow
- Lack of sleep (required amount of sleep may vary widely)
- Stress
Signs and symptoms
- Symptoms
- Vertigo: Spinning dizziness which is not light headed or off balance.
- Short duration (Paroxysmal): Lasts only seconds to minutes
- Positional in onset: only can be induced by a change in position.
- Nausea is often associated
- Visual disturbance: It may be difficult to read or see during an attack due to the associated nystagmus.
- Pre-Syncope (feeling faint) or Syncope (fainting) is unusual.
- Emesis (Vomiting) is uncommon but possible.
- Signs
- Rotatory (torsional) nystagmus, where the top of the eye rotates towards the affected ear and a beating or twitching fashion.
Patients do not experience other neurological deficits such as numbness or weakness, and if these symptoms are present, a more serious etiology such as posterior circulation stroke, must be considered.
Diagnosis
The condition is diagnosed from patient history (feeling of vertigo with sudden changes in positions); and by performing the Dix-Hallpike maneuver which is diagnostic for the condition. The test involves a reorientation of the head to align the posterior canal (at its entrance to the ampulla) with the direction of gravity. This test stimulus is effective in provoking the symptoms in subjects suffering from archetypal BPPV. These symptoms are typically a short lived vertigo, and observed nystagmus. In some patients, the vertigo can persist for years.
The nystagmus associated with BPPV has several important characteristics which differentiate it from other types of nystagmus.
- Positional: the nystagmus occurs only in certain positions
- Latency of onsent: there is a 5-10 second delay prior to onset of nystagmus
- Nystagmus lasts for 5-30 seconds
- Visual fixation does not suppress nystagmus due to BPPV
- Both a rotatory and upbeat vertical components are present
- The nystagmus beats in a geotrophic (top of the eye towards the ground fashion
- Repeated Dix-Hallpike maneuvers cause the nystagmus to fatigue or disappear temporarily
Treatment
Two treatments have been found effective for relieving symptoms of posterior canal BPPV: the canalith repositioning procedure (CRP) or Epley maneuver, and the liberatory or Semont maneuver.[1] The CRP employs gravity to move the calcium build-up that causes the condition.[3] The particle repositioning maneuver can be performed during a clinic visit by health professionals or taught to patients to practice at home. In the Semont maneuver, patients themselves are able to achieve canalith repositioning.[4] only limited data are available comparing the two treatments, and it is not known which is more effective.[1]
Devices such as a head over heels "rotational chair" are available at some tertiary care centers [5] Home devices, like the DizzyFIX, are also available for the treatment of BPPV and vertigo. [6][7]
The Epley maneuver (particle repositioning) does not address the actual presence of the particles (otoconia), rather it changes their location. The maneuver moves these particles from areas in the inner ear which cause symptoms, such as vertigo, and repositions them into areas where they do not cause these problems.
Meclizine is a commonly prescribed medication, but is ultimately ineffective for this condition, other than masking the dizziness. Other sedative medications help mask the symptoms associated with BPPV but do not affect the disease process or resolution rate. Betahistine (trade name Serc) is available in some countries and is commonly prescribed but again it is likely ineffective. Particle repositioning remains the current gold standard treatment for most cases of BPPV.
Surgical treatments, such as a semi-circular canal occlusion, do exist for BPPV but carry the same risk as any neurosurgical procedure. Surgery is reserved for severe and persistent cases which fail particle repositioning and medical therapy.
Migraine link
BPPV is one of the most common vestibular disorders in patients presenting with dizziness and migraine is implicated in idiopathic cases. Proposed mechanisms linking the two are genetic factors and vascular damage to the labyrinth.[8]
'연구하는 인생 > 西醫學 Medicine' 카테고리의 다른 글
| ★ Hippocratic Oath ★ 히포크라테스 선서 (0) | 2009.09.01 |
|---|---|
| Hyperlexia (0) | 2009.08.17 |
| Helicobacter (0) | 2009.07.06 |
| 高脂血症 [Hypercholesterolemia] (0) | 2009.06.18 |
| Dental braces (0) | 2009.04.29 |