Hypertension
| Hypertension | |
|---|---|
 Automated arm blood pressure meter showingarterial hypertension (shown a systolic blood pressure 158 mmHg, diastolic blood pressure99 mmHg and heart rate of 80 beats per minute) | |
| Classification and external resources | |
| Synonyms | arterial hypertension |
| Specialty | Cardiology |
| ICD-10 | I10,I11,I12, I13,I15 |
| ICD-9-CM | 401 |
| OMIM | 145500 |
| DiseasesDB | 6330 |
| MedlinePlus | 000468 |
| eMedicine | med/1106 ped/1097emerg/267 |
| Patient UK | Hypertension |
| MeSH | D006973 |
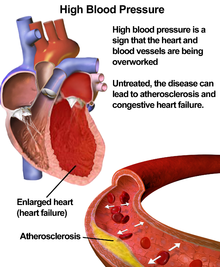
Hypertension (HTN or HT), also known as high blood pressure, is a long term medical conditionin which the blood pressure in the arteries is persistently elevated.[1] High blood pressure usually does not cause symptoms.[2] Long term high blood pressure; however, is a major risk factor forcoronary artery disease, stroke, heart failure, peripheral vascular disease, vision loss, and chronic kidney disease.[3][4]
High blood pressure is classified as either primary (essential) high blood pressure or secondary high blood pressure.[5] About 90–95% of cases are primary, defined as high blood pressure due to nonspecific lifestyle and genetic factors.[5][6] Lifestyle factors that increase the risk include excess salt, excess body weight, smoking, and alcohol.[2][5] The remaining 5–10% of cases are categorized as secondary high blood pressure, defined as high blood pressure due to an identifiable cause, such as chronic kidney disease, narrowing of the kidney arteries, an endocrine disorder, or the use of birth control pills.[5]
Blood pressure is expressed by two measurements, the systolic and diastolic pressures, which are the maximum and minimum pressures, respectively.[2] Normal blood pressure at rest is within the range of 100–140 millimeters mercury (mmHg) systolic and 60–90 mmHg diastolic.[7] High blood pressure is present if the resting blood pressure is persistently at or above 140/90 mmHg for most adults.[5] Different numbers apply to children.[8] Ambulatory blood pressure monitoring over a 24-hour period appears more accurate than office best blood pressure measurement.[1][5]
Lifestyle changes and medications can lower blood pressure and decrease the risk of health complications.[9] Lifestyle changes include weight loss, decreased salt intake, physical exercise, and a healthy diet.[5] If lifestyle changes are not sufficient blood pressure medications are used.[9]Up to three medications controls blood pressure in 90% of people.[5] The treatment of moderately high arterial blood pressure (defined as >160/100 mmHg) with medications is associated with an improved life expectancy.[10] The effect of treatment of blood pressure between 140/90 mmHg and 160/100 mmHg is less clear, with some reviews finding benefit[11][12] and others not finding benefit.[13] High blood pressure affects between 16 and 37% of the population globally.[5] In 2010 hypertension was believed to have been a factor in 18% (9.4 million) deaths.[14]
Signs and symptoms[edit]
Hypertension is rarely accompanied by any symptoms, and its identification is usually throughscreening, or when seeking healthcare for an unrelated problem. Some with high blood pressure report headaches (particularly at the back of the head and in the morning), as well aslightheadedness, vertigo, tinnitus (buzzing or hissing in the ears), altered vision or fainting episodes.[15] These symptoms, however, might be related to associated anxiety rather than the high blood pressure itself.[16]
On physical examination, hypertension may be associated with the presence of changes in the optic fundus seen by ophthalmoscopy.[17] The severity of the changes typical of hypertensive retinopathy is graded from I–IV; grades I and II may be difficult to differentiate.[17] The severity of the retinopathy correlates roughly with the duration and/or the severity of the hypertension.[15]
Secondary hypertension[edit]
Hypertension with certain specific additional signs and symptoms may suggest secondary hypertension, i.e. hypertension due to an identifiable cause. For example, Cushing's syndrome frequently causes truncal obesity, glucose intolerance, moon face, a hump of fat behind the neck/shoulder, and purple abdominal stretch marks.[18] Hyperthyroidism frequently causes weight loss with increased appetite, fast heart rate,bulging eyes, and tremor. Renal artery stenosis (RAS) may be associated with a localized abdominal bruit to the left or right of the midline (unilateral RAS), or in both locations (bilateral RAS). Coarctation of the aorta frequently causes a decreased blood pressure in the lower extremities relative to the arms, and/or delayed or absent femoral arterial pulses. Pheochromocytoma may cause abrupt ("paroxysmal") episodes of hypertension accompanied by headache, palpitations, pale appearance, and excessive sweating.[18]
Hypertensive crisis[edit]
Severely elevated blood pressure (equal to or greater than a systolic 180 or diastolic of 110) is referred to as a hypertensive crisis. Hypertensive crisis is categorized as either hypertensive urgency or hypertensive emergency, according to the absence or presence of end organ damage, respectively.[19][20]
In hypertensive urgency, there is no evidence of end organ damage resulting from the elevated blood pressure. In these cases, oral medications are used to lower the BP gradually over 24 to 48 hours.[21]
In hypertensive emergency, there is evidence of direct damage to one or more organs.[22][23] The most affected organs include the brain, kidney, heart and lungs, producing symptoms which may include confusion, drowsiness, chest pain and breathlessness.[21] In hypertensive emergency, the blood pressure must be reduced more rapidly to stop ongoing organ damage,[21] however, there is a lack of randomised controlled trial evidence for this approach.[23]
Pregnancy[edit]
Hypertension occurs in approximately 8–10% of pregnancies.[18] Two blood pressure measurements six hours apart of greater than 140/90 mm Hg is considered diagnostic of hypertension in pregnancy.[24] High blood pressure in pregnancy can be classified as pre-existing hypertension,gestational hypertension or pre-eclampsia.[25]
Pre-eclampsia is a serious condition of the second half of pregnancy and following delivery characterised by increased blood pressure and the presence of protein in the urine.[18] It occurs in about 5% of pregnancies and is responsible for approximately 16% of all maternal deathsglobally.[18] Pre-eclampsia also doubles the risk of perinatal mortality.[18] Usually there are no symptoms in pre-eclampsia and it is detected by routine screening. When symptoms of pre-eclampsia occur the most common are headache, visual disturbance (often "flashing lights"), vomiting, pain over the stomach, and swelling. Pre-eclampsia can occasionally progress to a life-threatening condition called eclampsia, which is ahypertensive emergency and has several serious complications including vision loss, brain swelling, seizures, kidney failure, pulmonary edema, and disseminated intravascular coagulation (a blood clotting disorder).[18][26]
In contrast, gestational hypertension is defined as new-onset hypertension during pregnancy without protein in the urine.[25]
Children[edit]
Failure to thrive, seizures, irritability, lack of energy, and difficulty breathing[27] can be associated with hypertension in neonates and young infants. In older infants and children, hypertension can cause headache, unexplained irritability, fatigue, failure to thrive, blurred vision, nosebleeds, andfacial paralysis.[27][28]
Causes[edit]
Primary hypertension[edit]
Hypertension results from a complex interaction of genes and environmental factors. Numerous common genetic variants with small effects on blood pressure have been identified[29] as well as some rare genetic variants with large effects on blood pressure.[30] Also, GWAS have identified 35 genetic loci related to blood pressure; 12 of these genetic loci influencing blood pressure were newly found.[31] Sentinel SNP for each new genetic loci identified has shown an association with DNA methylation at multiple nearby Cpg sites. These sentinel SNP are located within genes related to vascular smooth muscle and renal function. DNA methylation might affect in some way linking common genetic variation to multiple phenotypes even though mechanisms underlying these associations are not understood. Single variant test performed in this study for the 35 sentinel SNP (known and new) showed that genetic variants singly or in aggregate contribute to risk of clinical phenotypes related to high blood pressure.[31]
Blood pressure rises with aging and the risk of becoming hypertensive in later life is considerable.[32] Several environmental factors influence blood pressure. High salt intake raises the blood pressure in salt sensitive individuals; lack of exercise, obesity, stress,[16] and depression[33] can play a role in individual cases. The possible role of other factors such as caffeine consumption,[34] and vitamin D deficiency[35] are less clear.Insulin resistance, which is common in obesity and is a component of syndrome X (or the metabolic syndrome), is also thought to contribute to hypertension.[36] Events in early life, such as low birth weight, maternal smoking, and lack of breast feeding may be risk factors for adult essential hypertension, although the mechanisms linking these exposures to adult hypertension remain unclear.[37] An increased rate of high blood ureahas been found in untreated people with hypertensive in comparison with people with normal blood pressure, although it is uncertain whether the former plays a causal role or is subsidiary to poor kidney function.[38]
Secondary hypertension[edit]
Secondary hypertension results from an identifiable cause. Kidney disease is the most common secondary cause of hypertension.[18]Hypertension can also be caused by endocrine conditions, such as Cushing's syndrome, hyperthyroidism, hypothyroidism, acromegaly, Conn's syndrome or hyperaldosteronism, hyperparathyroidism and pheochromocytoma.[18][39] Other causes of secondary hypertension include obesity,sleep apnea, pregnancy, coarctation of the aorta, excessive liquorice consumption and certain prescription medicines, herbal remedies and illegal drugs.[18][40] Arsenic exposure through drinking water has been shown to correlate with elevated blood pressure.[41][42]
Pathophysiology[edit]
In most people with established essential hypertension, increased resistance to blood flow (total peripheral resistance) accounts for the high pressure while cardiac output remains normal.[43] There is evidence that some younger people with prehypertension or 'borderline hypertension' have high cardiac output, an elevated heart rate and normal peripheral resistance, termed hyperkinetic borderline hypertension.[44] These individuals develop the typical features of established essential hypertension in later life as their cardiac output falls and peripheral resistance rises with age.[44] Whether this pattern is typical of all people who ultimately develop hypertension is disputed.[45] The increased peripheral resistance in established hypertension is mainly attributable to structural narrowing of small arteries and arterioles,[46] although a reduction in the number or density of capillaries may also contribute.[47] Whether increased active arteriolar vasoconstriction plays a role in established essential hypertension is unclear.[48] Hypertension is also associated with decreased peripheralvenous compliance[49] which may increase venous return, increase cardiac preload and, ultimately, causediastolic dysfunction.
Pulse pressure (the difference between systolic and diastolic blood pressure) is frequently increased in older people with hypertension. This can mean that systolic pressure is abnormally high, but diastolic pressure may be normal or low — a condition termed isolated systolic hypertension.[50] The high pulse pressure in elderly people with hypertension or isolated systolic hypertension is explained by increased arterial stiffness, which typically accompanies aging and may be exacerbated by high blood pressure.[51]
Many mechanisms have been proposed to account for the rise in peripheral resistance in hypertension. Most evidence implicates either disturbances in the kidneys' salt and water handling (particularly abnormalities in the intrarenal renin-angiotensin system)[52] and/or abnormalities of the sympathetic nervous system.[53] These mechanisms are not mutually exclusive and it is likely that both contribute to some extent in most cases of essential hypertension. It has also been suggested that endothelial dysfunction and vascular inflammation may also contribute to increased peripheral resistance and vascular damage in hypertension.[54][55] Interleukin 17 has garnered interest for its role in increasing the production of several other immune system chemical signals thought to be involved in hypertension such as tumor necrosis factor alpha, interleukin 1, interleukin 6, and interleukin 8.[56]
Diagnosis[edit]
| System | Tests |
|---|---|
| Kidney | Microscopic urinalysis, protein in the urine, BUN and/or creatinine |
| Endocrine | Serum sodium, potassium, calcium, TSH |
| Metabolic | Fasting blood glucose, HDL, LDL, and total cholesterol, triglycerides |
| Other | Hematocrit, electrocardiogram, and chest radiograph |
| Sources: Harrison's principles of internal medicine[57] others[58][59][60][61][62] | |
Hypertension is diagnosed on the basis of a persistently high blood pressure. Traditionally, the National Institute of Clinical Excellence recommends three separate sphygmomanometer measurements at one monthly intervals.[63][64] The American Heart Association recommends at least three measurements on at least two separate health care visits.[65] Ambulatory blood pressure monitoring over 12 to 24 hours is the most accurate method to confirm the diagnosis.[66]
An exception to this is those with very high blood pressure readings especially when there is poor organ function.[64]Initial assessment of the hypertensive people should include a complete history and physical examination. With the availability of 24-hourambulatory blood pressure monitors and home blood pressure machines, the importance of not wrongly diagnosing those who have white coat hypertension has led to a change in protocols. In the United Kingdom, current best practice is to follow up a single raised clinic reading with ambulatory measurement, or less ideally with home blood pressure monitoring over the course of 7 days.[64] The United States Preventative Services Task Force also recommends getting measurements outside of the healthcare environment.[67] Pseudohypertension in the elderly or noncompressibility artery syndrome may also require consideration. This condition is believed to be due to calcification of the arteries resulting in abnormally high blood pressure readings with a blood pressure cuff while intra arterial measurements of blood pressure are normal.[68] Orthostatic hypertension is when blood pressure increases upon standing.[69]
Once the diagnosis of hypertension has been made, healthcare providers should attempt to identify the underlying cause based on risk factors and other symptoms, if present. Secondary hypertension is more common in preadolescent children, with most cases caused by kidney disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension.[70] Laboratory tests can also be performed to identify possible causes of secondary hypertension, and to determine whether hypertension has caused damage to the heart, eyes, and kidneys. Additional tests for diabetes and high cholesterol levels are usually performed because these conditions are additional risk factors for the development of heart disease and may require treatment.[6]
Serum creatinine is measured to assess for the presence of kidney disease, which can be either the cause or the result of hypertension. Serum creatinine alone may overestimate glomerular filtration rate and recent guidelines advocate the use of predictive equations such as theModification of Diet in Renal Disease (MDRD) formula to estimate glomerular filtration rate (eGFR).[71] eGFR can also provide a baseline measurement of kidney function that can be used to monitor for side effects of certain antihypertensive drugs on kidney function. Additionally, testing of urine samples for protein is used as a secondary indicator of kidney disease. Electrocardiogram (EKG/ECG) testing is done to check for evidence that the heart is under strain from high blood pressure. It may also show whether there is thickening of the heart muscle (left ventricular hypertrophy) or whether the heart has experienced a prior minor disturbance such as a silent heart attack. A chest X-ray or an echocardiogrammay also be performed to look for signs of heart enlargement or damage to the heart.[18]
Adults[edit]
| Category | systolic, mm Hg | diastolic, mm Hg |
|---|---|---|
| Normal | 90–119 | 60–79 |
| High normal[7] (Prehypertension) | 120–139 | 80–89 |
| Stage 1 hypertension | 140–159 | 90–99 |
| Stage 2 hypertension | 160–179 | 100–109 |
| Stage 3 hypertension[72][73] (Hypertensive emergency) | ≥180 | ≥110 |
| Isolated systolic hypertension | ≥140 | <90 |
In people aged 18 years or older hypertension is defined as a systolic and/or a diastolic blood pressure measurement consistently higher than an accepted normal value (currently 139 mmHg systolic, 89 mmHg diastolic: see table—Classification (JNC7)). Lower thresholds are used (135 mmHg systolic or 85 mmHg diastolic) if measurements are derived from 24-hour ambulatory or home monitoring.[64] Recent international hypertension guidelines have also created categories below the hypertensive range to indicate a continuum of risk with higher blood pressures in the normal range. JNC7 (2003)[71] uses the term prehypertension for blood pressure in the range 120–139 mmHg systolic and/or 80–89 mmHg diastolic, while ESH-ESC Guidelines (2007)[72] and BHS IV (2004)[73] use optimal, normal and high normal categories to subdivide pressures below 140 mmHg systolic and 90 mmHg diastolic. Hypertension is also sub-classified: JNC7 distinguishes hypertension stage I, hypertension stage II, and isolated systolic hypertension. Isolated systolic hypertension refers to elevated systolic pressure with normal diastolic pressure and is common in the elderly.[71] The ESH-ESC Guidelines (2007)[72] and BHS IV (2004)[73] additionally define a third stage (stage III hypertension) for people with systolic blood pressure exceeding 179 mmHg or a diastolic pressure over 109 mmHg. Hypertension is classified as "resistant" if medications do not reduce blood pressure to normal levels.[71]
Children[edit]
Hypertension occurs in around 0.2 to 3% of newborns; however, blood pressure is not measured routinely in healthy newborns.[28] Hypertension is more common in high risk newborns. A variety of factors, such as gestational age, postconceptional age and birth weight needs to be taken into account when deciding if a blood pressure is normal in a newborn.[28]
Hypertension defined as elevated blood pressure over several visits affects 1% to 5% of children and adolescents and is associated with long term risks of ill-health.[74] Blood pressure rises with age in childhood and, in children, hypertension is defined as an average systolic or diastolic blood pressure on three or more occasions equal or higher than the 95th percentile appropriate for the sex, age and height of the child. High blood pressure must be confirmed on repeated visits however before characterizing a child as having hypertension.[74] Prehypertension in children has been defined as average systolic or diastolic blood pressure that is greater than or equal to the 90th percentile, but less than the 95th percentile.[74] In adolescents, it has been proposed that hypertension and pre-hypertension are diagnosed and classified using the same criteria as in adults.[74]
The value of routine screening for hypertension in children over the age of 3 years is debated.[75][76] In 2004 the National High Blood Pressure Education Program recommended that children aged 3 years and older have blood pressure measurement at least once at every health care visit[74] and the National Heart, Lung, and Blood Institute and American Academy of Pediatrics made a similar recommendation.[77] However, theAmerican Academy of Family Physicians[78] support the view of the U.S. preventive Services Task Force that evidence is insufficient to determine the balance of benefits and harms of screening for hypertension in children and adolescents who do not have symptoms.[79]
Prevention[edit]
Much of the disease burden of high blood pressure is experienced by people who are not labeled as hypertensive.[73] Consequently, population strategies are required to reduce the consequences of high blood pressure and reduce the need for antihypertensive drug therapy. Lifestyle changes are recommended to lower blood pressure, before starting drug therapy. The 2004 British Hypertension Society guidelines[73] proposed the following lifestyle changes consistent with those outlined by the US National High BP Education Program in 2002[80] for the primary prevention of hypertension:
- maintain normal body weight for adults (e.g. body mass index 20–25 kg/m2)
- reduce dietary sodium intake to <100 mmol/ day (<6 g of sodium chloride or <2.4 g of sodium per day)
- engage in regular aerobic physical activity such as brisk walking (≥30 min per day, most days of the week)
- limit alcohol consumption to no more than 3 units/day in men and no more than 2 units/day in women
- consume a diet rich in fruit and vegetables (e.g. at least five portions per day);
Effective lifestyle modification may lower blood pressure as much as an individual antihypertensive drug. Combinations of two or more lifestyle modifications can achieve even better results.[73]
Management[edit]
According to one review published in 2003, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.[81]
Target blood pressure[edit]
Various expert groups have produced guidelines regarding how low the blood pressure target should be when a person is treated for hypertension. These groups recommend a target below the range 140-160 / 90-100 mmHg for the general population.[8][82][83][84][85]Controversy exists regarding the appropriate targets for certain subgroups, including the elderly, people with diabetes and people with kidney disease.[86]
Many expert groups recommend a slightly higher target of 150/90 mmHg for those over 80 years of age.[82][83][84] One expert group, the JNC-8, recommends the target of 150/90 mmHg for those over 60 years of age,[8] but some experts within this group disagree with this recommendation.[87] Some expert groups have also recommended slightly lower targets in those with diabetes[82] or chronic kidney disease with proteinuria,[88] but others recommend the same target as for the general population.[8][86] In 2015 a large trial suggests that among people over 50 with increased heart disease risk, aiming to reduce systolic blood pressure to 120 mmHg was associated with lower mortality but increased side effects compared to a target of 140 mmHg.[89]
Lifestyle modifications[edit]
The first line of treatment for hypertension is lifestyle changes, including dietary changes, physical exercise, and weight loss. Though these have all been recommended in scientific advisories,[90] a review by Cochrane found no evidence for effects of weight loss diets on death or long-term complications and adverse events in persons with hypertension.[91] The review did find a decrease in blood pressure.[91] Their potential effectiveness is similar to and at times exceeds a single medication.[7] If hypertension is high enough to justify immediate use of medications, lifestyle changes are still recommended in conjunction with medication.
Dietary changes shown to reduce blood pressure include diets with low sodium,[92] the DASH diet, vegetarian diets[93] and high potassium diets.[94]
Physical exercise regimens which are shown to reduce blood pressure include isometric resistance exercise, aerobic exercise, resistance exercise, and device-guided breathing.[95]
Stress reduction techniques such as biofeedback or transcendental meditation may be considered as an add-on to other treatments to reduce hypertension, but do not have evidence for preventing cardiovascular disease on their own.[95][96][97]
Medications[edit]
Several classes of medications, collectively referred to as antihypertensive medications, are available for treating hypertension.
First line medications for hypertension include thiazide-diuretics, calcium channel blockers, angiotensin converting enzyme inhibitors andangiotensin receptor blockers.[8] These drugs may be used alone or in combination; the latter option may serve to minimize counter-regulatory mechanisms that act to revert blood pressure values to pre-treatment levels.[8][98] The majority of people require more than one medication to control their hypertension.[90]
Resistant hypertension[edit]
Resistant hypertension is defined as hypertension that remains above goal blood pressure in spite of using, at once, three antihypertensive medications belonging to different drug classes. Low adherence to treatment is an important cause of resistant hypertension.[99] Resistant hypertension may also represent the result of chronic high activity of the autonomic nervous system; this concept is known as "neurogenic hypertension".[100]
Epidemiology[edit]
Adults[edit]
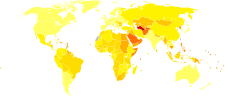
As of 2000, nearly one billion people or ~26% of the adult population of the world had hypertension.[102] It was common in both developed (333 million) and undeveloped (639 million) countries.[102] However, rates vary markedly in different regions with rates as low as 3.4% (men) and 6.8% (women) in rural India and as high as 68.9% (men) and 72.5% (women) in Poland.[103] In Europe hypertension occurs in about 30-45% of people as of 2013.[7]
In 1995 it was estimated that 43 million people in the United States had hypertension or were taking antihypertensive medication, almost 24% of the adult United States population.[104] The prevalence of hypertension in the United States is increasing and reached 29% in 2004.[105][106] As of 2006 hypertension affects 76 million US adults (34% of the population) and African American adults have among the highest rates of hypertension in the world at 44%.[107] It is more common in blacks and less in whites and Mexican Americans, rates increase with age, and is greater in the southeastern United States.[6][108] Hypertension is more common in men (though menopause tends to decrease this difference) and in those of lowsocioeconomic status.[6]
Children[edit]
Rates of high blood pressure in children and adolescents have increased in the last 20 years in the United States.[109] Childhood hypertension, particularly in preadolescents, is more often secondary to an underlying disorder than in adults. Kidney disease is the most common secondary cause of hypertension in children and adolescents. Nevertheless, primary or essential hypertension accounts for most cases.[110]
Outcomes[edit]
Hypertension is the most important preventable risk factor for premature death worldwide.[111] It increases the risk of ischemic heart disease[112] strokes,[18] peripheral vascular disease,[113] and other cardiovascular diseases, including heart failure, aortic aneurysms, diffuse atherosclerosis,chronic kidney disease, and pulmonary embolism.[18] Hypertension is also a risk factor for cognitive impairment and dementia.[18] Other complications include hypertensive retinopathy andhypertensive nephropathy.[71]
History[edit]
Measurement[edit]
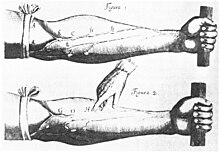
Modern understanding of the cardiovascular system began with the work of physician William Harvey (1578–1657), who described the circulation of blood in his book "De motu cordis". The English clergyman Stephen Hales made the first published measurement of blood pressure in 1733.[114][115] However hypertension as a clinical entity came into being in 1896 with the invention of the cuff-based sphygmomanometerby Scipione Riva-Rocci in 1896.[116] This allowed the measurement of blood pressure in the clinic. In 1905,Nikolai Korotkoff improved the technique by describing the Korotkoff sounds that are heard when the artery is ausculated with a stethoscope while the sphygmomanometer cuff is deflated.[115]
Identification[edit]
The symptoms similar to symptoms of patients with hypertensive crisis are discussed in medieval Persian medical texts in the chapter of "fullness disease".[117] The symptoms include headache, heaviness in the head, sluggish movements, general redness and warm to touch feel of the body, prominent, distended and tense vessels, fullness of the pulse, distension of the skin, coloured and dense urine, loss of appetite, weak eyesight, impairment of thinking, yawning, drowsiness, vascular rupture, and hemorrhagic stroke.[118] Fullness disease was presumed to be due to an excessive amount of blood within the blood vessels.
Descriptions of hypertension as a disease came among others from Thomas Young in 1808 and especially Richard Bright in 1836.[114] The first report of elevated blood pressure in a person without evidence of kidney disease was made by Frederick Akbar Mahomed (1849–1884).[119]
Treatment[edit]
Historically the treatment for what was called the "hard pulse disease" consisted in reducing the quantity of blood by bloodletting or the application of leeches.[114] This was advocated by The Yellow Emperor of China, Cornelius Celsus, Galen, and Hippocrates.[114] The therapeutic approach for the treatment of hard pulse disease included changes in lifestyle (staying away from anger and sexual intercourse) and dietary program for patients (avoiding the consumption of wine, meat, and pastries, reducing the volume of food in a meal, maintaining a low-energy diet and the dietary usage of spinach and vinegar).
In the 19th and 20th centuries, before effective pharmacological treatment for hypertension became possible, three treatment modalities were used, all with numerous side-effects: strict sodium restriction (for example the rice diet[114]), sympathectomy (surgical ablation of parts of thesympathetic nervous system), and pyrogen therapy (injection of substances that caused a fever, indirectly reducing blood pressure).[114][120]
The first chemical for hypertension, sodium thiocyanate, was used in 1900 but had many side effects and was unpopular.[114] Several other agents were developed after the Second World War, the most popular and reasonably effective of which were tetramethylammonium chloride,hexamethonium, hydralazine and reserpine (derived from the medicinal plant Rauwolfia serpentina). None of these were well tolerated[citation needed]. A major breakthrough was achieved with the discovery of the first well-tolerated orally available agents. The first waschlorothiazide, the first thiazide diuretic and developed from the antibiotic sulfanilamide, which became available in 1958.[114][121] Subsequentlybeta blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers and renin inhibitors were developed as antihypertensive agents.[120]
'연구하는 인생 > 西醫學 Medicine' 카테고리의 다른 글
| Prolotherapy, Proliferation therapy (0) | 2019.06.15 |
|---|---|
| How Dangerous Are CT Scans? (0) | 2014.10.14 |
| How Much Do CT Scans Increase the Risk of Cancer? (0) | 2014.10.14 |
| What are the risks and benefits of MRI? (0) | 2014.10.14 |
| CONNECTIVE TISSUE (0) | 2014.04.06 |