Trigeminal neuralgia
| Trigeminal neuralgia | |
|---|---|
| Classification and external resources | |
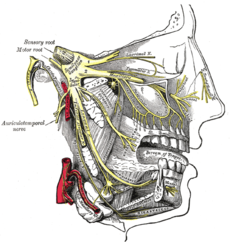 Detailed view of the trigeminal nerve and its three major divisions (shown in yellow): the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3) |
|
| ICD-10 | G50.0, G44.847 |
| ICD-9 | 350.1 |
| DiseasesDB | 13363 |
| eMedicine | emerg/617 |
| MeSH | D014277 |
Trigeminal neuralgia (TN, or TGN), tic douloureux[1] (also known as prosopalgia,[2] the Suicide Disease[3] or Fothergill's disease[4]) is a neuropathic disorder characterized by episodes of intense pain in the face, originating from the trigeminal nerve. It has been described as among the most painful conditions known to mankind.[5] It is estimated that 1 in 15,000 people suffer from TN, although the actual figure may be significantly higher due to frequent misdiagnosis. In a majority of cases, TN symptoms begin appearing after the age of 50, although there have been cases with patients being as young as three years of age. It is more common in females than males.[6]
The trigeminal nerve is a paired cranial nerve that has three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). one, two, or all three branches of the nerve may be affected. 10-12% of cases are bilateral (occurring on both the left and right sides of the face). Trigeminal neuralgia most commonly involves the middle branch (the maxillary nerve or V2) and lower branch (mandibular nerve or V3) of the trigeminal nerve,[7] but the pain may be felt in the ear, eye, lips, nose, scalp, forehead, cheeks, teeth, or jaw and side of the face.
TN is not easily controlled but can be managed with a variety of treatment options.[8]
Signs and symptoms
The disorder is characterized by episodes of intense facial pain that last from a few seconds to several minutes or hours. The episodes of intense pain may occur paroxysmally. To describe the pain sensation, patients may describe a trigger area on the face so sensitive that touching or even air currents can trigger an episode; however, in many patients the pain is generated spontaneously without any apparent stimulation. It affects lifestyle as it can be triggered by common activities such as eating, talking, shaving and brushing teeth. Wind, high pitched sounds, loud noises such as concerts or crowds, chewing, and talking can aggravate the condition in many patients. The attacks are said by those affected to feel like stabbing electric shocks, burning, pressing, crushing, exploding or shooting pain that becomes intractable.
Individual attacks usually affect one side of the face at a time, lasting from several seconds to a few minutes and repeat up to hundreds of times throughout the day. The pain also tends to occur in cycles with remissions lasting months or even years. 10-12% of cases are bilateral, or occurring on both sides. This normally indicates problems with both trigeminal nerves since one serves strictly the left side of the face and the other serves the right side. Pain attacks are known to worsen in frequency or severity over time, in some patients. Many patients develop the pain in one branch, then over years the pain will travel through the other nerve branches. Some patients also experience pain in the index finger.[9]
It may slowly spread to involve more extensive portions of the trigeminal nerve. The spread may even affect all divisions of the nerve, and sometimes simultaneously. Cases with bilateral involvement have not indicated simultaneous activity. The following suggest a systemic development: rapid spreading, bilateral involvement or simultaneous participation with other major nerve trunks. Examples of systemic involvement include multiple sclerosis or expanding cranial tumor. Examples of simultaneous involvement include tic convulsive (of the fifth and seventh cranial nerves) and occurrence of symptoms in the fifth and ninth cranial nerve areas.[10]
Outwardly visible signs of TN can sometimes be seen in males who may deliberately miss an area of their face when shaving, in order to avoid triggering an episode. Successive recurrences are incapacitating and the dread of provoking an attack may make sufferers unable to engage in normal daily activities.
Some patients report continuous pain or continuous pain during waking hours; for reasons that are not yet known, TN sufferers rarely have pain attacks or are awakened due to pain while they are sleeping. In fact, most patients have a very brief window of reprieve upon awakening from sleep, though that window can sometimes last only minutes. The mechanisms as to why one feels no pain while they are asleep, or in a slumber state, even though a pillow may be in contact with a "trigger point" on one's face, remains a mystery to physicians and dentists.
There is also a variant of TN called atypical trigeminal neuralgia (also referred to as "trigeminal neuralgia, type 2"),[11] based on a recent classification of facial pain.[12] In some cases of atypical TN the sufferer experiences a severe, relentless underlying pain similar to a migraine in addition to the stabbing shock-like pains. In other cases, the pain is stabbing and intense but may feel like burning or prickling, rather than a shock. Sometimes the pain is a combination of shock-like sensations, migraine-like pain and burning or prickling pain. It can also manifest as an unrelenting, boring, piercing pain.
Causes
The trigeminal nerve is a mixed cranial nerve responsible for sensory data such as tactition (pressure), thermoception (temperature), and nociception (pain) originating from the face above the jawline; it is also responsible for the motor function of the muscles of mastication, the muscles involved in chewing but not facial expression.
Several theories exist to explain the possible causes of this pain syndrome. It was once believed that the nerve was compressed in the opening from the inside to the outside of the skull; but newer leading research indicates that it is an enlarged blood vessel - possibly the superior cerebellar artery - compressing or throbbing against the microvasculature of the trigeminal nerve near its connection with the pons. Such a compression can injure the nerve's protective myelin sheath and cause erratic and hyperactive functioning of the nerve. This can lead to pain attacks at the slightest stimulation of any area served by the nerve as well as hinder the nerve's ability to shut off the pain signals after the stimulation ends. This type of injury may rarely be caused by an aneurysm (an outpouching of a blood vessel); by a tumor; by an arachnoid cyst in the cerebellopontine angle;[13] or by a traumatic event such as a car accident or even a tongue piercing.[14]
Short-term peripheral compression is often painless, with pain attacks lasting no more than a few seconds.[5] Persistent compression results in local demyelination with no loss of axon potential continuity. Chronic nerve entrapment results in demyelination primarily, with progressive axonal degeneration subsequently.[5] It is, "therefore widely accepted that trigeminal neuralgia is associated with demyelination of axons in the gasserion ganglion, the dorsal root, or both."[15] It has been suggested that this compression may be related to an aberrant branch of the superior cerebellar artery that lies on the trigeminal nerve.[15] Further causes, besides an aneurysm, multiple sclerosis or cerebellopontine angle tumor, include: a posterior fossa tumor, any other expanding lesion or even brainstem diseases from strokes.[15]
A large portion of multiple sclerosis patients have TN, but is not a symptom of MS. only two to four percent of patients with TN,[citation needed] usually younger,[citation needed] have evidence of multiple sclerosis, which may damage either the trigeminal nerve or other related parts of the brain. It has been theorized that this is due to damage to the spinal trigeminal complex.[16] Trigeminal pain has a similar presentation in patients with and without MS.[17]
Postherpetic Neuralgia, which occurs after shingles, may cause similar symptoms if the trigeminal nerve is damaged.
When there is no [apparent] structural cause, the syndrome is called idiopathic.
Management
As with many conditions without clear physical or laboratory diagnosis, TN is unfortunately sometimes misdiagnosed. A TN sufferer will sometimes seek the help of numerous clinicians before a firm diagnosis is made.
There is evidence that points towards the need to quickly treat and diagnose TN. It is thought that the longer a patient suffers from TN, the harder it may be to reverse the neural pathways associated with the pain.
The dentist must ensure a correct diagnosis does not mistake TN as a temporomandibular disorder.[18] Since triggering may be caused by movements of the tongue or facial muscles, TN must be differentiated from masticatory pain that has the clinical characteristics of deep somatic rather than neuropathic pain. Masticatory pain will not be arrested by a conventional mandibular local anesthetic block.[10]
Dentists who suspect TN should proceed in the most conservative manner possible and should ensure that all tooth structures are "truly" compromised before performing extractions or other procedures.
Medical
- The anticonvulsant carbamazepine is the first line treatment; second line medications include baclofen, lamotrigine, oxcarbazepine, phenytoin, gabapentin, and sodium valproate. Uncontrolled trials have suggested that clonazepam and lidocaine may be effective.[19]
- Low doses of some antidepressants such as amitriptyline are thought to be effective in treating neuropathic pain, but a tremendous amount of controversy exists on this topic, and their use is often limited to treating the depression that is associated with chronic pain, rather than the actual sensation of pain from the trigeminal nerve. Antidepressants are also used to counteract a medication side effect.
- Duloxetine can also be used in some cases of neuropathic pain, and as it is also an antidepressant can be particularly helpful where neuropathic pain and depression are combined. [20]
- Opiates such as morphine and oxycodone can be prescribed, and there is evidence of their effectiveness on neuropathic pain, especially if combined with gabapentin.[21][22]
Surgical
The evidence for surgical therapy is poor[23] and it is thus only recommended if medical treatment is not effective.[24] While there may be pain relief there is also frequently numbness post procedure.[23] Microvascular decompression appears to result in the longest pain relief.[23] Percutaneous radiofrequency thermorhizotomy may also be effective[25] as may gamma knife radiosurgery however the effectiveness decreases with time.[26]
Three other procedures use needles or catheters that enter through the face into the opening where the nerve first splits into its three divisions. Some have excellent success rates using a cost-effective percutaneous surgical procedure known as balloon compression have been reported.[27] This technique has been helpful in treating the elderly for whom surgery may not be an option due to coexisting health conditions. Balloon compression is also the best choice for patients who have ophthalmic nerve pain or have experienced recurrent pain after microvascular decompression.
Glycerol injections involve injecting an alcohol-like substance into the cavern that bathes the nerve near its junction. This liquid is corrosive to the nerve fibers and can mildly injure the nerve enough to hinder the errant pain signals. In a radiofrequency rhizotomy, the surgeon uses an electrode to heat the selected division or divisions of the nerve. Done well, this procedure can target the exact regions of the errant pain triggers and disable them with minimal numbness.
Notable cases
- Australian author Colleen McCullough has TN and has undergone surgical treatment in Jan 2010.[28]
- Entrepreneur and author Melissa Seymour was diagnosed with TN in 2009 and underwent microvascular decompression surgery in a well documented case covered by magazines and newspapers which helped to raise public awareness of the illness in Australia. Seymour was subsequently made a Patron of the Trigeminal Neuralgia Association of Australia.[29]
- Jim Fitzpatrick, the British Member of Parliament for Poplar and Limehouse disclosed that he was a sufferer from the condition when launching a Parliamentary debate on it on 27 July 2010.[30]
- Charles Sanders Peirce, who has been called "... the greatest American thinker ever,"[31] was a sufferer for most of his life.
- In August 2011, Indian actor Salman Khan disclosed that he has been suffering from trigeminal neuralgia for 7 years.[32] He had surgery for the condition in September 2011.[33]
- Jefferson Davis, the president of the Confederate States of America during the American Civil War also had TN. His first recorded attack was in 1852, when he was 44 years old, and he suffered from this ailment for the remainder of his life.[34]
See also
References
 |
| 삼차 신경통이란? | |||
| 제5 뇌신경으로도 불리는 삼차 신경에 생기는 신경통을 말합니다. 삼차 신경은 감각 및 운동 신경으로 된 혼합 신경이며, 이 신경의 역할은 안면, 구강, 코 점막, 혀의 촉각 등을 담당하며, 각막 및 결막 반사를 지배하고, 저작근(씹을 때 사용하는 근육)의 운동과 하악(아래턱)의 운동을 담당합니다. 그리고 눈물 및 침샘에서의 분비 작용을 담담하고 있습니다. 삼차신경통이란 얼굴의 감각을 담당하는 뇌신경인 삼차신경의 이상으로 인해서 얼굴 한쪽에 칼로 도려 내는 듯한 통증이나 전기감전으로 인한 통증이 발작적으로 순간적으로 1-수초간 나타나는 질병입니다. |
| 삼차 신경통은 왜 생기나요? | |||
| 가장 흔한 원인은 근육이나 인대(힘줄) 또는 뼈의 주변에서 통증을 담당하는 신경이 조여 있거나 신경으로 가는 혈액이 원활하지 못한 경우입니다. 그러므로 신경을 누르거나 신경으로 가는 혈관에 문제를 일으킬 수 있는 여러 가지 원인들이 모두 신경통을 유발시킬 수 있습니다. 즉, 뇌에서 두부에 12개의 뇌신경이 두경부의 신경을 장악하는데 이중 제5번 신경인 삼차신경이 뇌에서 나오는 부위에서 뇌혈관과 접촉에 의해서 만성적으로 신경이 자극되어 통증이 발생하는 경우가 대부분입니다. 이외에는 다발성신경경화증 등의 퇴행성 신경질환으로 발생하는 경우도 있습니다. 흔하지는 않지만 뇌종양에 의한 자극도 환자의 약 6~8%에서 발견되고 있습니다. |
| 삼차 신경통의 증상은? | |||
| 주로 40대 이후의 연령에서 자주 발생하며, 눈 주위에서 아래쪽으로 내려와 귀 뒷부분, 얼굴의 한쪽 면, 윗입술에까지 통증이 번지게 됩니다. 통증은 아주 심하여 가만히 있어도 아프고, 세수나 면도를 하거나, 음식물을 먹을 때 혹은 바람이 얼굴을 스쳐도 통증이 발생하고 살짝 건드려도 깜짝 놀랄 정도의 칼로 찌르는 듯한 심한 통증이 발생됩니다. 간혹 치통으로 오인되어 치과에서 발치를 하고 신경처리를 하지만 통증이 계속되는 환자도 있습니다. |
| 삼차 신경통은 어떻게 치료하나요? | |||
| 일단 통증 발작이 일어날 때에는 가급적 잘대 안정을 취하고, 주위 환경을 어둡게 하며, 소음을 차단 하여 조용한 상태를 유지하는 것이 도움이 됩니다. 일반적인 진통제로는 호전되지 않을 정도로 통증이 심해 항 간질 약물을 사용하며, 만일 약물 치료로 효과가 없는 경우에는 수술적 치료나 신경차단법으로 효과를 보기도 합니다. 삼차 신경통의 통증은 너무나 격심하기 때문에 보통 진통제로는 진통이 되지 않고 항경련약인 테그레톨, 페니토인과 바클로펜 등을 많이 사용합니다. 기타 수술요법은 현미경하에서 뇌 속의 삼차신경을 압박하고 있는 혈관을 박리 유리시키는 방법으로 발달 되어 있습니다. 신경차단술은 삼차 신경의 세가지 가지와 그로부터 나온 말초신경가지의 필요한 부분만을 찾아 들어가 신경차단 약물을 투여하는 것입니다. |
| 생활 가이드 | |||
| 통증이 있으면 무리를 하지 말고 휴양을 하도록 합니다. 아픈 부위를 차갑게 하지 않도록 하고, 커피, 알코올, 담배, 향신료 따위의 자극이 강한 음식물의 섭취를 피하고, 비타민류가 풍부한 식품을 먹도록 힘씁니다 |
'연구하는 인생 > 西醫學 Medicine' 카테고리의 다른 글
| Hemorrhagic Stroke (0) | 2012.06.18 |
|---|---|
| Varicose veins 정맥류 varix varices (0) | 2012.05.27 |
| migraine 편두통 (0) | 2012.05.25 |
| Smell (0) | 2012.05.08 |
| Snapping Scapula Syndrome (0) | 2012.04.21 |